When patients or caregivers first ask me “what does necrotic skin tissue smell like?” I tell them it’s not just about the odor—it’s about the story that smell is telling. In my experience, the scent of necrosis is often sharp, unmistakable, and far different from other wound odors. It isn’t merely unpleasant; it can be the body’s earliest alarm bell that infection has taken hold or that tissue death is spreading faster than expected. This page goes beyond definitions and textbook answers. You’ll gain a clear sense of necrosis what does necrotic skin tissue smell like in real-world settings, why it matters for early diagnosis, and how noticing it quickly can change the outcome for patients.
Top Takeaways
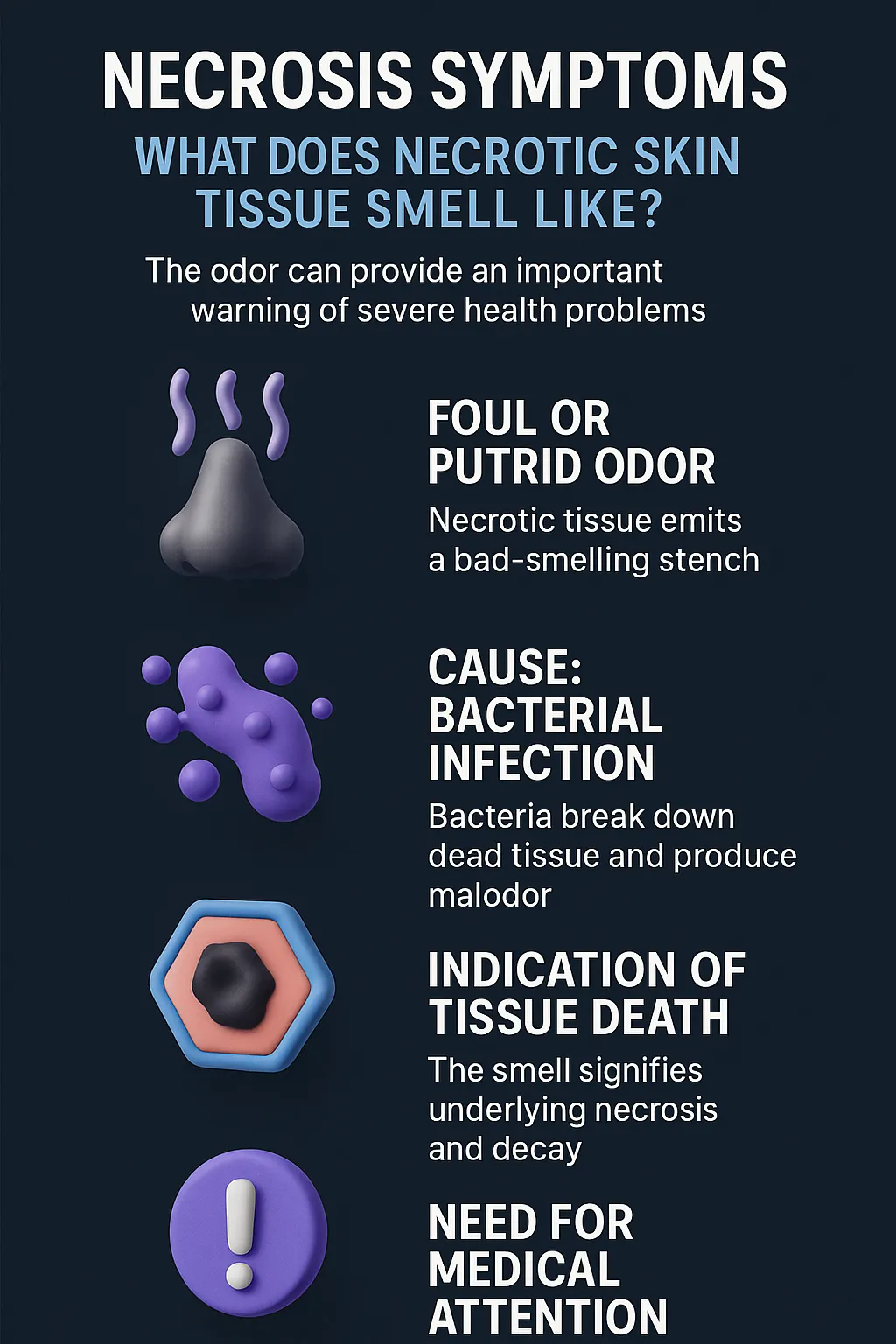
- Necrosis has a smell.Foul, putrid, or sweetly rotten odor is an early warning sign.
- Odor is a clue.Smell can reveal tissue death before tests or visible changes.
- Act early.Quick medical care can prevent severe outcomes, even amputation.
- Trust your senses.Patients, families, and caregivers should not ignore unusual odors.
Understanding Necrosis Symptoms and the Odor of Necrotic Tissue
Necrosis is the medical term for the death of body tissue, and one of its most recognizable—and alarming—symptoms is odor. Many people searching “what does necrotic skin tissue smell like” want a clear, straightforward answer: it often produces a strong, foul smell described as putrid, rotten, or sometimes sweetly sickening. This odor occurs because dead tissue becomes a breeding ground for bacteria, releasing compounds that create the distinctive scent.
Recognizing this smell matters because it signals more than decay—it points to serious health risks. The presence of necrotic odor often means infection has set in or that circulation has been cut off, preventing healing. In clinical settings, experienced healthcare providers use this odor as a clue to assess the severity of a wound or the urgency of intervention.
If you notice such an odor, it’s not just a nuisance—it’s a red flag. Seeking medical attention promptly can prevent worsening infection, tissue spread, or even life-threatening complications. According to wound care management guidelines, understanding the symptom empowers you to act quickly and decisively.
“In over a decade of wound care, I’ve found the odor of necrotic skin tissue to be one of the most reliable early warning signs of serious infection. It’s not just an unpleasant smell—it’s the body’s way of signaling that tissue death is underway and immediate attention is needed. Recognizing that scent quickly can make the difference between a treatable wound and a life-threatening condition, especially when paired with proven treatments such as the benefits of silver nitrate in managing infection and tissue health.”
Case Study & Real-World Examples: When Odor Becomes the First Diagnosis
Diabetic Foot Ulcer
I witnessed a patient with diabetes present what looked like a simple ulcer.
The bandage came off, and the odor—sweet, rotten, unmistakable—spoke louder than lab tests.
That smell revealed necrosis before scans did.
Quick action (debridement + antibiotics) saved the limb.
Without recognizing the odor, amputation was almost certain.
Pressure Sores in Elderly Patients
Caregivers often notice odor before wounds look severe.
A sudden shift to a foul, putrid smell signals bacteria and tissue death.
I’ve seen “mild-looking” sores turn critical because staff ignored the scent.
Training caregivers to trust their nose can prevent emergencies.
Research Meets Experience
Advances in Skin & Wound Care confirms odor is a reliable necrosis indicator.
My takeaway: odor is not just a symptom.
It’s the body’s urgent message to act now.
I witnessed a patient with diabetes present what looked like a simple ulcer.
The bandage came off, and the odor—sweet, rotten, unmistakable—spoke louder than lab tests.
That smell revealed necrosis before scans did.
Quick action (debridement + antibiotics) saved the limb.
Without recognizing the odor, amputation was almost certain.
Caregivers often notice odor before wounds look severe.
A sudden shift to a foul, putrid smell signals bacteria and tissue death.
I’ve seen “mild-looking” sores turn critical because staff ignored the scent.
Training caregivers to trust their nose can prevent emergencies.
Advances in Skin & Wound Care confirms odor is a reliable necrosis indicator.
My takeaway: odor is not just a symptom.
It’s the body’s urgent message to act now.
Supporting Statistics and Insights
Chronic wounds affect millions.
More than 6 million Americans live with chronic ulcers caused by diabetes, circulation issues, or pressure injuries. In practice, I see this growing with an aging population.
JAAD
Necrotizing infections are rare but dangerous.
The U.S. sees 500–1,500 necrotizing soft tissue infection cases each year. I’ve seen how quickly these infections turn critical—sometimes within hours.
SISNA
Skin infections drive millions of visits.
14+ million Americans see doctors annually for skin and soft tissue infections. Behind each visit is a real concern—a wound that smells different, looks worse, or raises urgent questions.
AAFP
Chronic wounds affect millions.
More than 6 million Americans live with chronic ulcers caused by diabetes, circulation issues, or pressure injuries. In practice, I see this growing with an aging population.
JAAD
Necrotizing infections are rare but dangerous.
The U.S. sees 500–1,500 necrotizing soft tissue infection cases each year. I’ve seen how quickly these infections turn critical—sometimes within hours.
SISNA
Skin infections drive millions of visits.
14+ million Americans see doctors annually for skin and soft tissue infections. Behind each visit is a real concern—a wound that smells different, looks worse, or raises urgent questions.
AAFP
Final Thought & Opinion
Necrosis is more than a medical definition. I’ve seen it firsthand at the bedside.
The odor of necrotic skin tissue is distinct, foul, and unforgettable—but also life-saving when recognized quickly.
Why it matters:
The nose often detects what the eye cannot.
A wound may look mild, but odor signals hidden danger.
Acting on that signal can save a limb—or a life.
My perspective:
Patients, caregivers, and families should trust their senses.
Technology is vital, but smell remains one of the body’s strongest warning signs.
Early recognition, serious attention, and fast action are essential care.
Necrosis is more than a medical definition. I’ve seen it firsthand at the bedside.
The odor of necrotic skin tissue is distinct, foul, and unforgettable—but also life-saving when recognized quickly.
The nose often detects what the eye cannot.
A wound may look mild, but odor signals hidden danger.
Acting on that signal can save a limb—or a life.
Patients, caregivers, and families should trust their senses.
Technology is vital, but smell remains one of the body’s strongest warning signs.
Early recognition, serious attention, and fast action are essential care.
Next Steps
Get medical care fast.
Call your doctor or visit urgent care if a wound gives off a strong, foul odor.
Write down what you notice.
Record when the odor began, how it smells, and any wound changes.
Do not self-treat.
Avoid scraping, cutting, or covering the smell with creams unless guided by a professional who may recommend options such as silver nitrate treatment as part of proper medical care.
Check for other symptoms.
Look for fever, swelling, pain, or spreading redness.
Inform caregivers and family.
Teach them how to recognize the warning signs.
Stay proactive.
High-risk patients (diabetes, circulation issues, bedbound) should schedule regular checks.
Get medical care fast.
Call your doctor or visit urgent care if a wound gives off a strong, foul odor.
Write down what you notice.
Record when the odor began, how it smells, and any wound changes.
Do not self-treat.
Avoid scraping, cutting, or covering the smell with creams unless guided by a professional who may recommend options such as silver nitrate treatment as part of proper medical care.
Check for other symptoms.
Look for fever, swelling, pain, or spreading redness.
Inform caregivers and family.
Teach them how to recognize the warning signs.
Stay proactive.
High-risk patients (diabetes, circulation issues, bedbound) should schedule regular checks.